Patient With History of Acute Steroid-Dependent Skin GVHD Develops Chronic GVHD: Part 1
Presentation
A 67-year-old male has a prior history of myelofibrosis that transformed into acute myeloid leukemia. Following induction with liposomal daunorubicin and cytarabine, along with a bone marrow biopsy that revealed remission, the patient underwent allogeneic stem cell transplantation with a haplo-identical donor.
Post-Transplant Course
The patient’s conditioning consisted of fludarabine, cyclophosphamide, and total body irradiation and post-transplant cyclophosphamide on days 3 and 4 post-transplant. Mycophenolate mofetil (MMF) was added on days 5 through 35 and tacrolimus started on day 5 and continued for GVHD prophylaxis. His immediate post-transplant course was complicated by grade II GI toxicity with diarrhea and nausea, which improved upon engraftment, and a transient rash that resolved without interventions prior to hospital discharge.
The patient developed mild erythema on the back on day 22, for which triamcinolone cream 0.1% strength was started. The patient then presented on day 29 with pruritic, maculopapular erythematous rash across the back, front, chest, abdomen, bilateral arms, and head, sparing the lower body and just under 50% body surface area (stage II acute GVHD of the skin according to Mount Sinai Acute GVHD International Consortium [MAGIC] criteria).1 At that time the patient also had two to three loose stools per day which were not watery, not associated with the timing of food, and without abdominal cramping.
The patient also reported slight ocular sensitivity to light (photophobia) at that time.
Workup
A skin punch biopsy was performed on day 29. It revealed a superficial perivascular infiltrate of lymphocytes with interface change and scattered dyskeratotic keratinocytes, predominantly in the follicular epithelium interface dermatitis, which were consistent with GVHD. It was also noted that the biopsy specimen had epithelial disorganization consistent with prior cytotoxic chemotherapy treatment.
An acute GVHD onset panel with GVHD biomarkers ST2 and regenerating islet-derived 3-alpha (REG3α) were obtained and revealed a medium risk of severe acute GvHD and non-relapse mortality (NRM).2
- REG3α 30
- ST2 111,997
- aGvHD algorithm 0.283
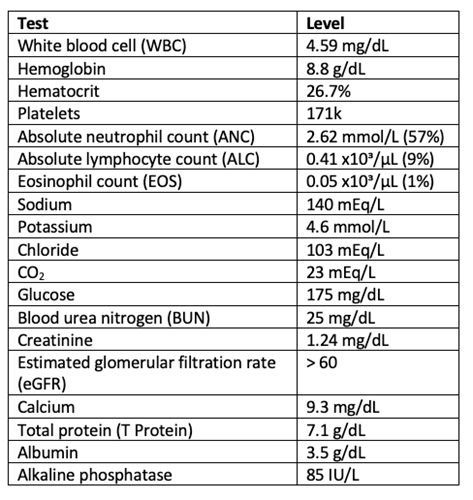
The patient also had the following lab results on day 29.
Treatment
The patient was started on high-dose prednisone at 1 mg/kg (80 mg) on day 29 post-transplant and tacrolimus was continued. Mycophenolate mofetil was continued three times daily through day 35 and significant improvement in the rash was noted. As prednisone began to be tapered, the patient developed recurrence of his rash. Due to the recurrence of acute GVHD on the steroid taper requiring an increase in the steroid dose and the inability to taper further, the patient was diagnosed as steroid-dependent and ruxolitinib was ordered.3 The patient started ruxolitinib 10 mg twice daily on day 61. Due to below-normal renal function, high lactate dehydrogenase (LDH), and low platelet count, the decision was made to switch from tacrolimus to sirolimus. Over time, prednisone continued to be tapered successfully to 10 mg daily.
At approximately day 110, the patient developed skin itching and a rash with normal LFTs and no GI symptoms. On day 118 the rash was worsened despite therapeutic sirolimus levels, prednisone 10 mg daily, and ruxolitinib 10 mg twice daily. Because of the lichenoid appearance of the rash, the patient was felt to have chronic GVHD features, and given a skin score 2 on the National Institutes of Health (NIH) Consensus chronic GVHD scoring. The patient was switched from ruxolitinib to ibrutinib at 420 mg at that time.4 Insurance authorization was obtained for extracorporeal photopheresis, but this was not needed. The skin rash improved to score 1 (using NIH criteria) with ibrutinib but absolute neutrophil count trended down while on the medication, so the dose was reduced to 280 mg daily. Sirolimus was tapered over 3 months and ibrutinib was also successfully discontinued at approximately 8 months post-transplant.
Discussion
GVHD is considered steroid-dependent if any of the following are present: (1) there is a partial response by day 56 of initial therapy; (2) the patient is steroid sensitive, but still receiving >10 mg/m2 per day of prednisone by day 56 (averaged over 2 days and assessed within a ±3-day window from day 56); (3) the patient is steroid sensitive, but still receiving steroids beyond day 80 of acute GVHD treatment; or (4) there is a flare requiring a ≥25% increase in steroid dose without the addition of other new systemic therapies for acute GvHD before the onset of chronic GvHD.5
Acute and chronic GVHD used to be categorized based on whether they occurred <100 or ≥ 100 days post-transplant, but they are now categorized based on clinical characteristics.6 Currently approved medications to treat chronic GVHD include ibrutinib, ruxolitinib, and belumosudil. Multiple other medications are in the pipeline.
To be continued in the next case presentation.
References
- Harris AC, Young R, Devine S, et al. International, multicenter standardization of acute graft-versus-host disease clinical data collection: A report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transplant. 2016;22(1):4-10. doi:10.1016/j.bbmt.2015.09.001
- Major-Monfried H, Renteria AS, Pawarode A, et al. MAGIC biomarkers predict long-term outcomes for steroid-resistant acute GVHD. Blood. 2018;131(25):2846-2855. doi:10.1182/blood-2018-01-822957
- Jagasia M, Perales MA, Schroeder MA, et al. Ruxolitinib for the treatment of steroid-refractory acute GVHD (REACH1): a multicenter, open-label phase 2 trial. Blood. 2020;135(20):1739-1749. doi:10.1182/blood.2020004823
- Rahmat LT, Logan AC. Ibrutinib for the treatment of patients with chronic graft-versus-host disease after failure of one or more lines of systemic therapy. Drugs Today (Barc). 2018;54(5):305-313. doi:10.1358/dot.2018.54.5.2807865
- El Jurdi N, Rayes A, MacMillan ML, et al. Steroid-dependent acute GVHD after allogeneic hematopoietic cell transplantation: risk factors and clinical outcomes. Blood Adv. 2021;5(5):1352-1359. doi:10.1182/bloodadvances.2020003937
- Jagasia MH, Greinix HT, Arora M, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21(3):389-401.e1. doi:10.1016/j.bbmt.2014.12.001