Elevated Bilirubin Following Engraftment: Differentiating SOS/VOD From GVHD
Transplant and Follow-Up
A 24-year-old Hispanic female with relapsed high-risk acute myeloid leukemia underwent a pre-transplant workup, which was significant for high ferritin/iron overload from persistent transfusion needs prior to transplant. She received busulfan/cyclophosphamide conditioning followed by graft-versus-host disease (GVHD) prophylaxis including post-transplant cyclophosphamide and tacrolimus/mycophenolate mofetil. She had a matched unrelated donor who was a major ABO mismatch. Both the patient and donor were cytomegalovirus and Epstein-Barr virus seropositive.
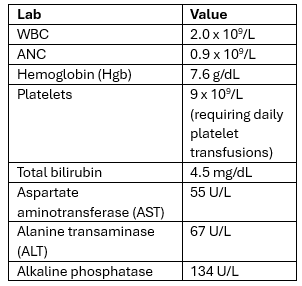
The patient’s post-transplant course was initially unremarkable, aside from grade 1/2 GI toxicity with nausea, vomiting, and small-volume diarrhea, which resolved by day +14. White blood cell (WBC) engraftment occurred on day +18 with absolute neutrophil count (ANC) >0.5 x3 days. On day +19, the patient was found to have right upper quadrant abdominal pain in the setting of weight increase. On exam, she had fluid wave and her liver was tender, palpable below the costal margin. The patient did not have rash or diarrhea. Her weight up-trended from a baseline of 146 lb to 154 lb between days +18 and +21. Her lab workup at this time showed the following:
Doppler ultrasound of the abdomen revealed hepatomegaly and reversal of portal flow.
In the setting of elevated bilirubin and recent engraftment, the differential in this patient included liver involvement of GVHD as well as sinusoidal obstructive syndrome (SOS)/veno-occlusive disease (VOD). A transjugular biopsy of the liver revealed extensive dilatation and congestion of sinusoids, intraluminal deposition of extracellular matrix with entrapped erythrocytes, and inflammation and deposition of fibrous tissue.¹ This liver biopsy, along with the overall clinical picture, was more consistent with SOS/VOD than GVHD.
Treatment
The patient was given defibrotide 6.25 mg/kg every 6 hours starting on day +21, and this was continued through day +43. The patient’s platelet transfusion needs improved over time, and bilirubin improved to 1.2. Ascites also improved.
Discussion
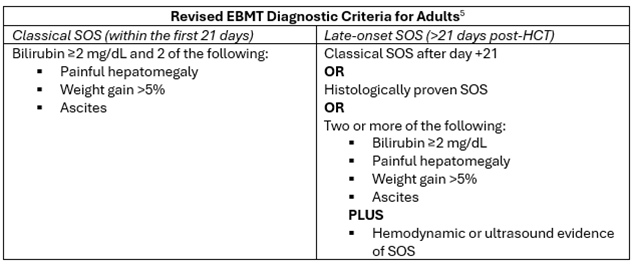
SOS, formerly known as VOD, is a rare, potentially life-threatening complication of hematopoietic cell transplant (HCT) that carries a very high mortality in severe cases (>80%).2 Due to the high potential for progression to multi-organ dysfunction (renal and pulmonary toxicity), an awareness among advanced practice providers in the field of allogeneic HCT is very important. Clinicians are encouraged to keep a high clinical suspicion. Traditionally, diagnosis of SOS/VOD has been based on the Baltimore (1987) or modified Seattle criteria (updated from the original 1984 Seattle Criteria), but additional sensitivity and specificity has been added in the more recently revised European Society for Blood and Marrow Transplantation (EBMT) criteria.3-5
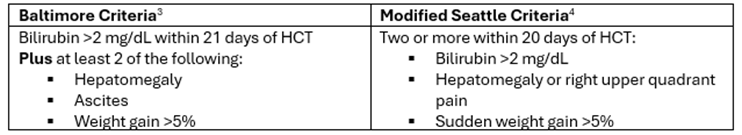
In the revised EBMT diagnostic criteria for adults, addition of the late-onset SOS category and additional histologic and imaging findings allow for inclusion of patients beyond day +21 as follows:
Risk factors for SOS/VOD include the following:
- Transplant-related factors
- Unrelated donor
- HLA-mismatched donor
- Non–T-cell–depleted graft
- Myeloablative conditioning regimen
- Oral or high-dose busulfan-based regimen
- High-dose total-body irradiation–based regimen
- Having a second HCT
- Patient- and disease-related factors
- Older age
- Lower Karnofsky score (<90%)
- Metabolic syndrome
- Females receiving norethisterone
- Advanced disease (beyond second complete response or relapsed/refractory)
- Thalassemia
- Certain genetic factors
- Hepatic-related factors
- Elevated transaminases >2.5x upper limit of normal (ULN)
- Serum bilirubin >1.5 ULN
- Cirrhosis
- Active viral hepatitis
- Abdominal or hepatic irradiation
- Previous history of receiving gemtuzumab ozogamicin or inotuzumab ozogamicin
- Hepatoxic drugs
- Iron overload/elevated ferritin level5
Hepatic GVHD can be difficult to diagnose when considering the broad differential diagnoses for elevated bilirubin, alkaline phosphatase, AST, and ALT. The Mount Sinai Acute GVHD Consortium—commonly referred to as the “MAGIC” criteria paper from 2016—states that liver GVHD alone is not diagnosed when bilirubin levels are elevated prior to the diagnosis of GVHD in another target organ and do not increase further, in the absence of liver biopsy confirmation.6 Other potential causes included are chemotherapy toxicity, sinusoidal obstructive syndrome, and parenteral nutrition-associated cholestasis. That being said, “it is important to document and diagnose the presence of liver GVHD due to the poorer prognosis it portends.”6
A liver biopsy in a case like this patient can be invaluable to help understand whether steroids are needed in addition to defibrotide. Liver biopsies in patients with hepatic GVHD may show many different changes involving interlobular bile ducts, including nuclear and cytoplasmic abnormalities, dysmorphic bile ducts, apoptosis, and cholangiocyte necrosis, among others.7 Liver biopsy remains the gold standard in diagnosis of hepatic involvement of GVHD.
This patient remained on defibrotide until there was resolution of hepatomegaly, elevated bilirubin, and improvement in her platelet transfusion needs over 3 weeks, at which time the defibrotide was discontinued. Defibrotide, the only FDA-approved medication for the treatment of SOS/VOD, is dosed at 6.25 mg/kg every 6 hours IV for 21-60 days, until SOS resolution or hospital discharge.8 Usually ursodiol is continued during treatment. Defibrotide should be started promptly upon the recognition and diagnosis of SOS/VOD due to the high mortality in these patients.
Studies are ongoing in the search for identifying more specific biomarkers, and a recent study reports that elevated serum autotaxin (ATX) levels may be predictive for the development and mortality associated with severe SOS/VOD.9 Additionally, prophylaxis with defibrotide is being studied and has shown efficacy.2,10 Cost analysis and discussion of this technique was presented in the 2024 Tandem Meetings of the American Society for Transplantation and Cellular Therapy and the Center for International Blood and Marrow Transplant Research.11 Ongoing attention to these data will likely be helpful over time.
References
- Fan CQ, Crawford JM. Sinusoidal obstruction syndrome (hepatic veno-occlusive disease). J Clin Exp Hepatol. 2014;4:332-346.
- Mohty M, Malard F, Abecasis M, et al. Prophylactic, preemptive, and curative treatment for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a position statement from an international expert group. Bone Marrow Transplant. 2020;55:485-495.
- Jones RJ, Lee KS, Beschorner WE, et al. Venoocclusive disease of the liver following bone marrow transplantation. Transplantation. 1987;44:778-783.
- McDonald GB, Sharma P, Matthews DE, et al. Venoocclusive disease of the liver after bone marrow transplantation: diagnosis, incidence, and predisposing factors. Hepatology. 1984;4:116-122.
- Mohty M, Malard F, Abecassis M, et al. Revised diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a new classification from the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant. 2016;51:906-912.
- Harris AC, Young R, Devine S, et al. International, Multicenter Standardization of Acute Graft-versus-Host Disease Clinical Data Collection: A Report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transplant. 2016;22:4-10.
- Stueck AE, Fiel MI. Hepatic graft-versus-host disease: What we know, when to biopsy, and how to diagnose. Hum Pathol. 2023;141:170-182.
- DEFITELIO (defibrotide sodium) prescribing information. Jazz Pharmaceuticals; Dublin, Ireland. 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208114lbl.pdf
- Takemura K, Nakamae M, Okamura H, et al. Autotaxin is a potential predictive marker for the development of veno-occlusive disease/sinusoidal obstruction syndrome after allogeneic hematopoietic cell transplantation. Ann Hematol. 2024;103:1705-1715.
- Chalandon Y, Mamez AC, Giannotti F, et al. Defibrotide shows efficacy in the prevention of sinusoidal obstruction syndrome after allogeneic hematopoietic stem cell transplantation: A retrospective study. Transplant Cell Ther. 2022;28:765.e1-765.
- Mohty M, Duncan C. Cancelling the cascade of VOD/SOS: Team-based prophylaxis, diagnosis, and customized management. Presented at: Tandem Meetings, Transplant & Cellular Therapies Meetings of ASTCT and CIBMTR; February 21, 2024; San Antonio, Texas. https://tandem.confex.com/tandem/2024/meetingapp.cgi/Session/8105