CRS and Acute Skin GVHD Responsive to Steroids in a Complicated Post-transplant Course
Presentation
A 60-year-old male has a history of recurrent follicular lymphoma that has transformed to large cell lymphoma. The patient was initially on a regimen including pentostatin, cyclophosphamide, and rituximab and had a good treatment response with near resolution of disease. Nine months later, the patient had progression of disease and was given bendamustine for 6 months. He did well, but unfortunately relapsed approximately 13 months later. He completed 6 cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) and was in remission for 3 years until he relapsed again.
The patient was given another several cycles of bendamustine plus rituximab but did not have a complete response. He was then given idelalisib, which was discontinued due to toxicity with diarrhea and cough. The patient presented again with disease progression approximately 13 months later and the biopsy showed that he had diffuse large B-cell lymphoma. He was given salvage RICE (rituximab, ifosfamide, carboplatin, and etoposide) with a partial response.
This was followed by an unsuccessful attempt to mobilize autologous stem cells. Due to the lack of other available options, the decision was made to proceed to allogeneic hematopoietic cell transplantation (alloHCT). No sibling or human leukocyte antigen (HLA)-matched unrelated donors were available so the patient’s haploidentical daughter was used as peripheral blood stem cell donor.
Post-transplant Course
The transplant conditioning regimen included fludarabine, cyclophosphamide, and total body irradiation, while post-transplant GVHD prophylaxis consisted of cyclophosphamide and tacrolimus/mycophenolate mofetil (MMF). The patient’s immediate post-transplant course was complicated by hectic neutropenic fevers and altered mental status resembling cytokine release syndrome (CRS) starting around day +11 post-transplant.
He also had concurrent acute kidney injury with creatinine as high as 2.8, which led to tacrolimus being switched to sirolimus. The patient was treated with IV steroids which improved both the fevers and mental status and he was weaned off steroids over approximately 5 days. Following this, he developed grade 3 mucositis and nausea and vomiting.
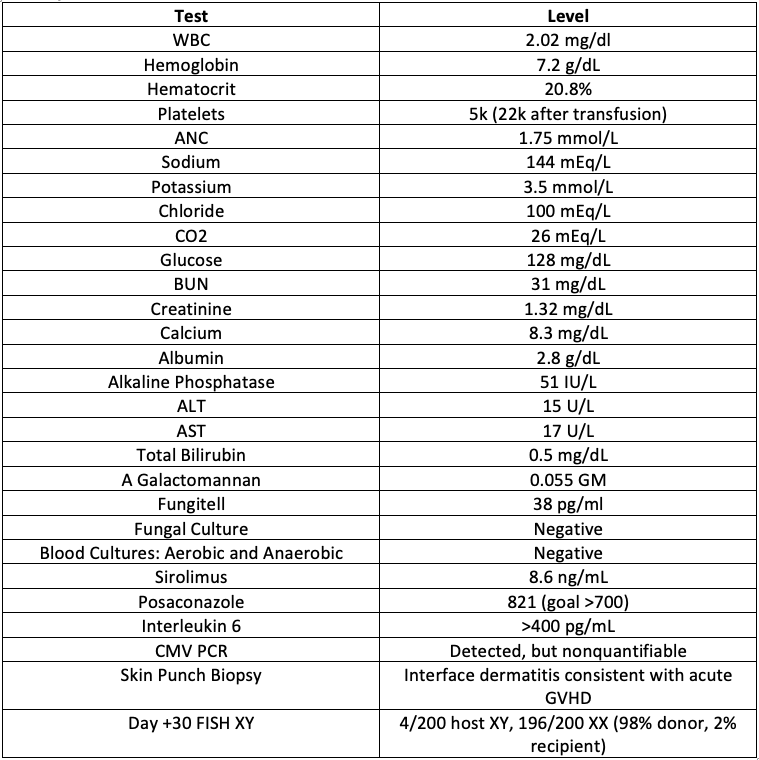
At the time of engraftment, which was approximately day +19 post-transplant, the patient developed an erythematous, maculopapular rash which extended across the patient’s entire back, chest, and abdomen, as well as the bilateral arms. According to the Wallace Rule of Nines, the rash extended across approximately 54% of the body surface area. The patient was also having recurrent fevers and an extensive infectious workup (see chart) was negative aside from the cytomegalovirus (CMV) PCR test where the viral infection was detected as non-quantifiable.
Workup
Treatment and Follow-up
Due to stage 3 acute GVHD of the skin, the patient was started on prednisone at 1 mg/kg per day and continued on sirolimus at therapeutic levels. The patient’s skin rash improved on prednisone over subsequent weeks, but he developed CMV viremia and required antiviral treatment and readmission and had continued cytopenias. Thankfully, the GVHD continued to be controlled and the prednisone was successfully tapered over 10 weeks and discontinued. No additional GVHD treatment was required.
A repeat chimerism test at day +60 post-transplant in the form of FISH XY improved to 1/200 cells XY, 199/200 XX (99.5% donor). At day +100 post-transplant, chimerism improved to all 200 XX (100% donor) and a PET CT revealed no evidence of residual lymphoma. The patient also did not develop chronic GVHD.
Discussion
This patient developed both CRS and stage 3 skin and overall clinical grade 2 acute GVHD according to the Mount Sinai Acute GVHD International Consortium (MAGIC) criteria.1
CRS is a systemic inflammatory response with abnormal immune activation and immune hyperstimulation which leads to cytokine levels being increased and a large amount of inflammation in the body.
Advanced practice providers in transplant and cellular therapy may be more familiar with CRS following CAR-T cell infusions. However, recent studies have analyzed CRS in haploidentical-related donor transplantation (haplo-HCT) and found that patients who presented CRS developed grade 2-4 acute GVHD more frequently than those who did not.2 Additionally, severe CRS was more common with peripheral blood vs. bone marrow grafts. Having CRS also was associated with lower relapse rates.3
Among risk factors for development of acute GVHD, the most important is HLA mismatch. Other risk factors include sex disparity between donor and recipient, increased age of the donor or the recipient, multiparous female donor, ineffective GVHD prophylaxis, intensity of the conditioning regimen, and peripheral blood stem cells rather than bone marrow grafts.4
This patient had a very high-risk disease, which was not in remission at the time of his alloHCT. He also had mixed chimerism results, with remaining male circulating blood cells at day +30 and day +60 post-transplant, which eventually improved to being 100% donor. In addition, he had a CMV infection beginning at the time of his initiation on high-dose steroids, which then required antivirals which worsened his blood counts. High dose steroids increase the risk of both infection and primary malignant disease relapse, so the goal is to minimize the amount of steroids used and taper as tolerated to avoid any prolonged exposures unless they are necessary. It is very fortunate that he responded to steroids and was able to be weaned off of them without requiring additional GVHD treatment.
References
- Harris AC, Young R, Devine S, et al. International, Multicenter Standardization of Acute Graft-versus-Host Disease Clinical Data Collection: A Report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transplant. 2016;22(1):4-10.
- Solán L, Landete E, Bailén R, et al. Cytokine release syndrome after allogeneic stem cell transplantation with posttransplant cyclophosphamide. Hematol Oncol. 2020;38(4):597-603.
- Abboud R, Wan F, Mariotti J, et al. Cytokine release syndrome after haploidentical hematopoietic cell transplantation: an international multicenter analysis. Bone Marrow Transplant. 2021;56(11):2763-2770.
- Aladağ E, Kelkitli E, Göker H. Acute Graft-Versus-Host Disease: A Brief Review. Turk J Haematol. 2020;37(1):1-4.