First Relapse of Multiple Myeloma Patient
Presentation
This is a 64-year-old male with a history of lambda light chain proteinuria, ISS stage II initially diagnosed with multiple myeloma in 2004. He completed induction therapy on the upfront phase II clinical trial with single agent bortezomib. Dexamethasone was added at cycle 4 due to progression, and thalidomide was added at cycle 7 for ongoing progression. He then underwent cyclophosphamide mobilization, followed by an autologous peripheral blood stem cell transplant a month later conditioned with melphalan 200 mg/m2. He achieved a partial remission at day 100 restaging and was offered a second transplant at that time, which he declined. He was then started on thalidomide maintenance, developing peripheral neuropathy, and in 2007 maintenance was changed to lenalidomide.
He did well with stable residual disease for close to 19 years until 2023 at which time he began to have a rise in his lambda light chain to 316 mg/L and urine paraprotein 259 mg/24hr. He also noted new back pain, although he remained very active. PET/CT demonstrated a new L3 lytic lesion with imaging otherwise negative. Bone marrow biopsy notes 25% plasma cells with FISH and cytogenetics neg. Labs note a normal WBC, hemoglobin 12.2 gm/dL, hematocrit 37%, platelets within normal range, BUN 30 mg/dL, and creatinine 2.37 mg/dL. Other comorbidities include chronic kidney disease (CKD) stage G3a/A2, renal osteodystrophy, hypertension, grade 1 peripheral neuropathy to hands and feet, and mild anemia.
Treatment
This case is different in that our patient is having his first relapse 19 years out from starting initial myeloma treatment and the treatment landscape looks very different today. In looking at the National Comprehensive Cancer Network (NCCN) guidelines for approaches to first relapse, there are many treatment options for this patient.1 Standard of care includes at least one agent from a different class or more potent from the same class. Triple combinations are preferred and considerations include an anti-CD38, proteasome inhibitor (PI) plus dexamethasone, anti-CD38 plus immunomodulatory agent (IMiD) plus dexamethasone or a PI, IMiD plus dexamethasone. You would also want to consider his risk status and other comorbidities, as well as a potential clinical trial. Currently, he is progressing on lenalidomide maintenance which has been an easy regimen for this very active patient. His disease remains standard risk per his latest restaging.
We reviewed the available treatments and options for our patient and decided on a regimen of daratumumab, pomalidomide, and dexamethasone. While we spent time on all the available options and recommendations, one of the most challenging issues for this patient has been the relapse itself. Our patient has been doing well for years on a single agent maintenance that has had little impact on his quality of life for about 19 years. He has had stable residual disease for so long, he feels that this relapse is worse than his original diagnosis. How as clinicians do we support our patient through the psychosocial challenges of relapse while still moving forward with the needed treatment?
As for the treatment, we started daratumumab, pomalidomide 4 mg, and weekly dexamethasone at 20 mg. We monitored his blood counts carefully and started him on an antiviral and a bone agent renally adjusted. He continued on his daily 81 mg aspirin for DVT prophylaxis. From the disease standpoint, he responded quickly with a reduction in his urine paraprotein back to 0 mg/24hr after 3 months and his free lambda light chain reduced to 9.1 mg/L. His anemia resolved and his kidney function improved back to his baseline. The psychosocial issues took a little more time and did improve with response to treatment and reduction in the dexamethasone dosing. Our patient also started counseling to help with his anxiety related to relapse and the changes of going from an oral maintenance drug to a multidrug regimen.
Discussion
Daratumumab is an IgG anti CD38-directed monoclonal antibody (mAB) and has shown to be as effective as monotherapy though especially effective in combination regimens for relapsed or refractory or newly diagnosed myeloma.2 While daratumumab was initially intravenous, the subcutaneous formulation has a similar safety profile and significantly fewer infusion-related issues.3 The most common grade 3 or 4 adverse events were neutropenia, anemia, and thrombocytopenia in the daratumumab plus pomalidomide and dexamethasone arm. Infection-related issues were also reported in this arm with pneumonia and lower respiratory tract infections.2 Daratumumab is an IgG antibody and can be detected on both serum protein electrophoresis and immunofixation so a type and screen should be obtained prior to dosing. Hepatitis B serologies should also be obtained prior to dosing and monitored throughout. When used in combination with an IMiD, all prescribers and patients must adhere to the REMS program.4
Pomalidomide is an analogue of thalidomide and is used as a single agent or in combination therapy. Patients on IMiDs are at increased risk for venous thromboembolism (VTE) and need to be on prophylaxis based on the assessment of underlying risk factors. Based on clinical trials, neuropathy was seen in about 18% of patients.5 Overall, the combination of daratumumab, pomalidomide, and dexamethasone has shown to be effective in a patient previously exposed to bortezomib and refractory to lenalidomide.2,6 The dosing schedule for daratumumab is once weekly on days 1, 8, 15, and 22 for the first 2 cycles, then every other week for cycles 3-6, and then monthly thereafter. Pomalidomide typically is 4 mg by mouth for 21 out of 28 days. Dexamethasone is usually 20 or 40 mg by mouth weekly and tapered down as indicated.
The other treatment aspect to consider with a relapsed patient and a new regimen is how to meet the psychological and psychosocial needs of the patient. With our patient, this first relapse was more challenging to him than his diagnosis. Psychosocial considerations have been a component of cancer care for over 25 years. The NCCN established a panel of oncologists, nurses, social workers, clergy, psychiatrists, and psychologists back in 1997 to develop guidelines related to distress screening. They also published a report in 2007 discussing “Cancer Care for the Whole Patient” which further elaborated on the guidelines and recommended a model that included distress screening, psychosocial needs, treatment, referral plans, and an evaluation.7
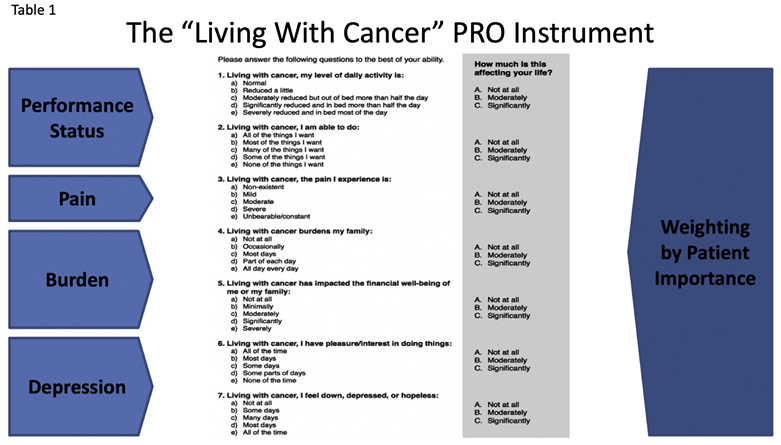
With myeloma patients living longer, attention is needed on both symptom and disease control as well as on the psychological impact. Psychosocial intervention should be introduced to myeloma patients early and throughout treatment.8 A tool such as the patient-reported outcomes (PRO) tool has been reported to help. In the pilot study at a single institution, they used a 7-item PRO tool to assess symptom burden and then went on to study with multiple centers. The results show that physical and psychological distress and financial and social concerns continue to be problematic for patients. Specific to myeloma patients, they had concerns about the inability to do things they want to do, financial burdens, lack of pleasure, pain, depression, impact on family, and ability to perform daily activities. The study shows an association between high levels of stress and decreased survival.9 (Table 1)
This case is an example of relapse following a long period of response and the impact to the patient. There are so many treatment options at this point and the APP has a role in both the next line of therapy and in ongoing assessment of the impact from a psychosocial standpoint. More literature is needed, although there is data to suggest that a high level of distress does correlate to poor outcomes.
References
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Multiple Myeloma. Version 2.2024, 11/01/23 © 2023. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.nccn.org/professionals/physician_gls/pdf/myeloma.pdf
- Dimopoulos MA, Terpos E, Boccadoro M, et al. Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma (APOLLO): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(6):801-812. doi:10.1016/S1470-2045(21)00128-5
- Mateos MV, Nahi H, Legiec W, et al. Subcutaneous versus intravenous daratumumab in patients with relapsed or refractory multiple myeloma (COLUMBA): a multicentre, open-label, non-inferiority, randomised, phase 3 trial [published correction appears in Lancet Haematol. 2020 Oct;7(10):e710]. Lancet Haematol. 2020;7(5):e370-e380. doi:10.1016/S2352-3026(20)30070-3
- Janssen Biotech, Inc. (2023) DARZALEX® (daratumumab) injection package insert and prescribing information. http://www.janssenlabels.com/package-insert/product-monograph/, and prescribing information. https://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/DARZALEX-pi.pdf
- Bristol-Myers Squibb Company (2023). POMALYST (pomalidomide) package insert. https://www.pomalysthcp.com/
- Devarakonda S, Sharma N, Efebera Y. The first relapse in multiple myeloma: how to pick the next best thing. Hematology Am Soc Hematol Educ Program. 2022;2022(1):560-568. doi:10.1182/hematology.2022000356
- Zabora J, Buzaglo J, Kennedy V, et al. Clinical perspective: Linking psychosocial care to the disease continuum in patients with multiple myeloma. Palliat Support Care. 2015;13(4):829-838. doi:10.1017/S1478951514000649
- Lamers J, Hartmann M, Goldschmidt H, Brechtel A, Hillengass J, Herzog W. Psychosocial support in patients with multiple myeloma at time of diagnosis: who wants what? Psychooncology. 2013;22(10):2313-2320. doi:10.1002/pon.3284
- Richter J, Sanchez L, Biran N, et al. Prevalence and Survival Impact of Self-Reported Symptom and Psychological Distress Among Patients With Multiple Myeloma. Clin Lymphoma Myeloma Leuk. 2021;21(3):e284-e289. doi:10.1016/j.clml.2020.11.021