Patient Diagnosed With Polycythemia Vera After Presenting With Iron Deficiency and Leukocytosis
Presentation
Mrs. T is a pleasant and friendly 66-year-old female with a medical history significant for hypothyroidism, combined systolic or diastolic heart failure, atrial fibrillation, alcohol-induced acute pancreatitis, gastric bypass, depression, and insomnia. Her PCP notes that she has iron deficiency and leukocytosis and refers her to hematology for further evaluation and workup.
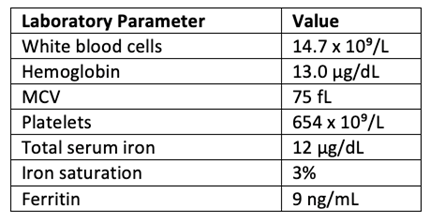
Labs performed by PCP include the following:
At her initial visit with hematology, Mrs. T reports that the leukocytosis was noted during a recent occurrence of pancreatitis and subsequent cardiac complications and thought to be related to these acute events. Additionally, regarding iron deficiency, she reports taking oral iron for a time, which improved iron stores. She has not taken iron supplementation for the past 2 months.
Workup
Mrs. T reports fatigue, especially when climbing stairs, and overall feelings of inactivity. She also notes difficulty concentrating, intermittent night sweats, and pruritus. She denies early satiety, weight loss, and current abdominal discomfort.
Labs performed at initial hematology consultation include the following:

*Flow cytometry on peripheral blood is negative for high-grade hematological malignancy.
Discussion After Initial Visit
The PA reviews the results of the initial workup with Mrs. T, which include persistent elevation of white blood cells with the presence of immature granulocytes, no blasts. Platelets remain elevated, so the PA explains that persistent thrombocytosis of this degree is more likely due to underlying primary bone marrow disorder than iron deficiency. The PA also discusses with Mrs. T that even though she is iron deficient, her red blood cells are increased, and current hematocrit levels may not be a true representation of true red blood cell volume given severe microcytosis secondary to iron deficiency.
Given the lab results and concern for masked polycythemia vera (PV), the PA asks Mrs. T to return to the lab for a repeat complete blood count (CBC), erythropoietin level, and JAK2. JAK2 mutation testing can be performed on the peripheral blood and can be an initial step in identifying the presence of a myeloproliferative neoplasm.
Additional Workup
CBC is unchanged, erythropoietin is low-normal at 3.7 mlU/mL, and JAK2 is positive for V617F mutation.
Mrs. T is advised to have a bone marrow aspiration and biopsy to support the diagnosis and for further assessment of cytogenetics and full molecular next-generation sequencing (NGS) panel.
Her bone marrow biopsy shows hypercellular marrow (95%) with panhyperplasia and megakaryocytic atypia and no reticulin fibrosis, diploid cytogenetics, and JAK2 positivity, remaining NGS negative.
Mrs. T’s MPN 10 score is 26. She reports fatigue, inactivity, difficulty concentrating, night sweats, and pruritus.
Diagnosis and Treatment
The PA discusses with Mrs. T that the above workup supports a diagnosis of PV. Conventional risk factors for high-risk PV include age >60 or history of thrombotic events; therefore, she is started on cytoreductive therapy. The PA and Mrs. T discuss several treatment options including hydroxyurea, pegylated interferons, and ruxolitinib. Given the potential for mood alterations with interferons and current uncontrolled depression, hydroxyurea is chosen as front-line therapy. The PA discusses with Mrs. T that she may have better symptom control with ruxolitinib and that they would continue to assess the need for a therapy change overtime.
For thrombosis prevention, Mrs. T is already taking apixaban due to atrial fibrillation, and with her history of gastric bypass, she is not advised to take aspirin, so she continues apixaban.
Discussion
This case is a great reminder that during initial workup of abnormal labs, advanced practice providers need to consider a broad differential. In a patient referred with leukocytosis and thrombocytosis, reactive causes are most likely; however, the persistence of these elevated counts should raise concern for underlying hematological malignancy. Additionally, hemoglobin and hematocrit levels, while typically considered for a diagnosis of PV, are not always elevated to the degree needed based on World Health Organization criteria.1 Masked PV is difficult to detect, but in patients with severe iron deficiency and microcytosis, consideration of red blood cell number becomes increasingly important.
Reference
- Barbui T, Thiele J, Gisslinger H, et al. The 2016 WHO classification and diagnostic criteria for myeloproliferative neoplasms: document summary and in-depth discussion. Blood Cancer J. 2018;8:15.
